Q&A with Dr. Lisa Butterfield, PhD: Cancer Vaccines & Adoptive Cell Transfer
Dr. Lisa Butterfield, PhD recently joined the Parker Institute for Cancer Immunotherapy as Vice President focusing on cell therapies while she continues her independent cancer vaccine research as an Adjunct Professor of Microbiology and Immunology at the University of California, San Francisco. She also sits on the Executive Committee and Board of Directors for the Society for Immunotherapy of Cancer (SITC) and shared with us her views on the future of cancer vaccines.
NS: What led to your interest in immuno-oncology?
LB: In junior high, I was interested in gene therapy and intrigued by the idea of replacing defective genes to cure diseases which eventually led me to cancer immunology. Learning about the complexities of the immune system– its specificity, its durability, and its capacity to evolve over time– struck me as both incredibly elegant and important. Applying that understanding of the immune system toward antigens within cancer was one of the most important and fascinating areas for me to be involved in as a scientist.
NS: What excites you about your recent move to the Parker Institute for Cancer Immunotherapy?
LB: It’s the caliber of science and the degree of collaboration that I’m most excited about. My time in Pittsburgh as the Director of Immunologic Monitoring and Cellular Product Lab showed me the power of people working together to accomplish bench-to-bedside research. During my time in leadership at the SITC I had the opportunity to see the current state of the field, where it was heading, and watch the early development of the Parker Institute model. The Parker Institute takes some of the best science in the field and unites people in an environment of open sharing to facilitate research progress. Projects routinely include biotech, biopharma, and academics to expedite answers to important questions. This decreases time spent in siloed research where people quietly reinvent the wheel at their individual institution. This model of connectivity, incredible science, clinical translation, and collaboration was the most impactful setting I could imagine for science.
NS: How did you first learn about NanoString?
LB: I was at a SITC meeting, talking about immunotherapy biomarkers and trying to understand the best way to ask gene expression questions in precious human samples. I was sitting next to someone much smarter, better experienced, and more famous than me who then looked over at me and said under her breath, “NanoString” in a way that told me that she already knew that this technology was a good way forward.
NS: How would you describe your experience working with NanoString to create the content for the Chimeric Antigen Receptor T cell (CAR-T) Characterization Panel?
LB: I’ve been at the table with different members of NanoString, often through SITC, working together on biomarker task forces, creating best practice white papers, and looking at high throughput data. I also had the opportunity to set up a collaboration on a cancer vaccine trial where I could take advantage of the NanoString nCounter® PanCancer Pathways and PanCancer Immune Gene Expression Panels. When I heard there would be a new panel around T cell biology and CAR-T cells in particular, I joined the opportunity not only to try the new tool but also to have input on shaping it moving forward.
NS: How do cancer vaccines work? In what key ways are they different from other cancer immunotherapies such as checkpoint inhibition?
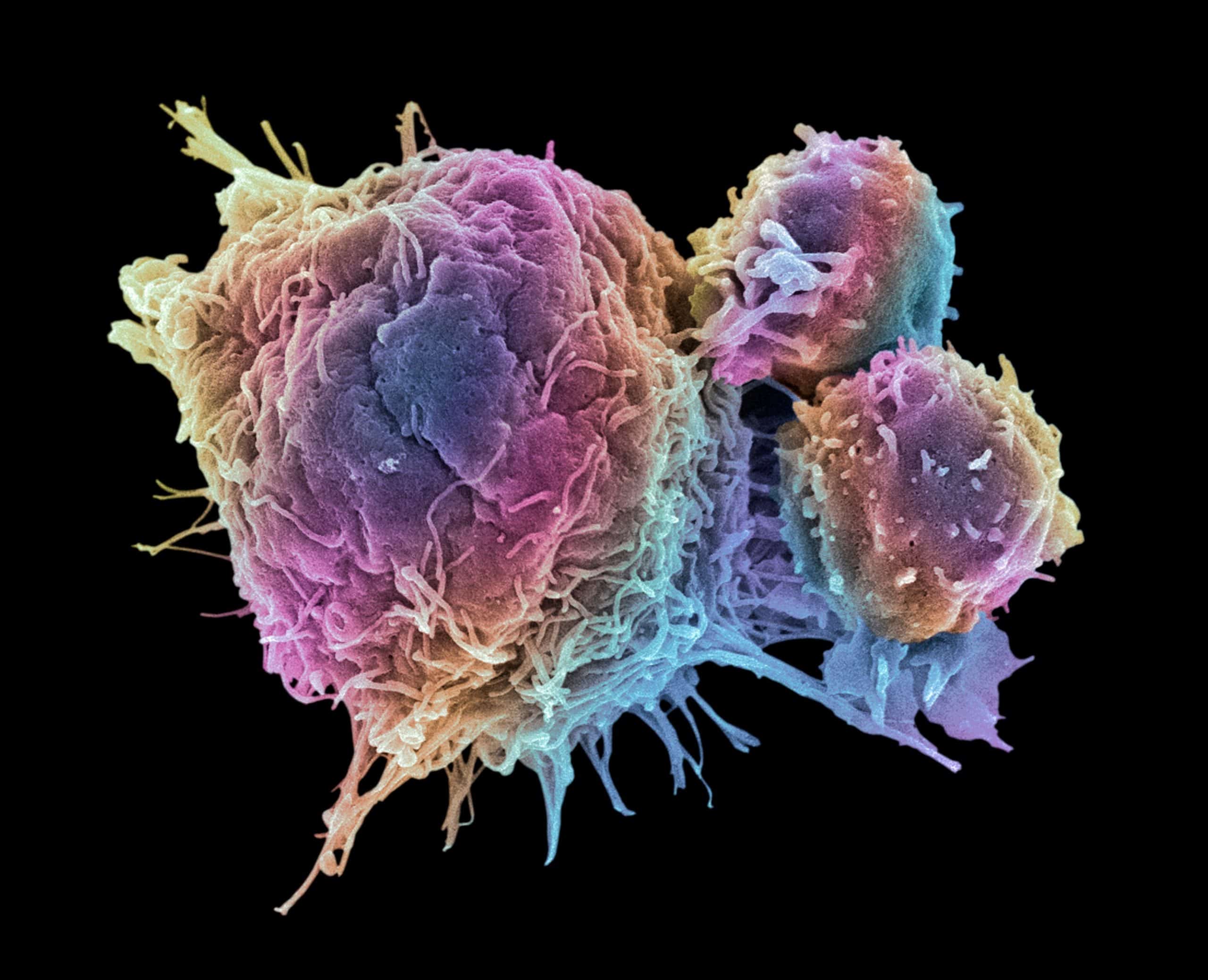
LS: Checkpoint inhibition capitalizes on existing crosstalk between the tumor and the immune system. These tumors have become edited, T cells have been exhausted, immune suppression is in effect, and regulatory T cells increased in number. The checkpoint inhibition therapies work in different ways to help reverse immune suppression and reinvigorate partially exhausted T cells. Cancer vaccines, on the other hand, are designed to promote T cells that are lacking by delivering tumor antigen in an immunogenic way to promote the T cell response. This may prime new T cell responses, boost existing low-level responses, or activate existing T cells that were either not activated or not proliferating sufficiently. Cancer vaccines promote and broaden T cell immune responses which then set the stage for amplification and shaping by the checkpoint blockade, additional co-stimulation triggers, or other therapeutics.
NS: The cancer vaccine mechanism of action seems to be similar to adoptive cell therapy or CAR-T cell therapy. Is one method superior to the other or can they be complementary?
LB: Cancer vaccines work with the existing T cell repertoire that can be limited by T cell deletion, skewing, or exhaustion. The vaccine alone may not be potent enough to reinvigorate them. Adoptive transfer can use tumor-infiltrating lymphocytes that are already native to the patient and the tumor; they’ve just been amplified and reinvigorated in culture ex vivo. The limitation of TIL is that the endogenous repertoire may not be potent enough or may be limited in antigen specificity. CAR-T and TCR engineering can eliminate some of the existing T cell defects, but at the cost of often limited antigenic breadth. There are strengths and weaknesses to all these approaches, but I hope they will continue to evolve together as personalized medicine. In the future, I imagine we can take a tumor biopsy, profile it, and determine what that particular patient needs and how their tumor is likely to respond. Then we can administer a bolus of T cells, a vaccine, or both, and then combine it with a checkpoint inhibitor to activate the T cell clones potent enough to overcome immune suppression.
NS: What are some of the biggest challenges in adoptive T cell therapy?
LB: After years of effort, we know how to genetically engineer and expand T cells. Now we need to know how to make them persist even longer, traffic to and infiltrate an immunosuppressive tumor microenvironment, and eliminate unintended toxicity. There’s a lot of clever engineering to be done, especially if we can eliminate the dependency on the viral vectors currently used. Having non-viral methods will allow us to test potential therapies much faster.
NS: What other immune cells are promising targets for adoptive cell therapy?
LB: While every immune cell has a positive and negative side, I’d look at effector cells that might be able to partner with T cells or take over when a T cell is no longer effective. Macrophages or natural killer (NK) cells are appealing; cells that are capable of killing targets and have entirely different mechanisms of target recognition will be important avenues to pursue.
NS: How far has allogeneic CAR-T cell therapy progressed? Will it eventually supplant autologous CAR-T cells?
LB: In an autologous system, we don’t need to know all the signals in a fine level of detail because everything is matched to that patient’s own tumor. The promise of an off-the-shelf, allogenic cell transfer is exciting but it’s going to be a much tougher engineering question to know what needs to be modulated to have allogeneic cells be effective over longer periods of time. Getting an allogeneic T cell to persist without unintended toxicity is challenging. What we learn about signal from autologous cell transfer will inform the approach to allogeneic cells.
NS: Is there a disadvantage to treating a patient who has already has their immune system challenged by other treatments such as radiation or chemotherapy? What about using adoptive cell therapy as the first line of treatment?
LB: We’re still learning about the risk/benefit ratio for patients and so for safety reasons this is not yet a first-line treatment. Consider the case of cancer vaccination—it used to be limited to a Stage 4 setting. It then turned out to be so safe and immunogenic that it is now being tested in prevention settings on patients with pre-malignant disease that are at a high risk for developing cancer. I think that adoptive cell therapies will follow that same path once we have a better understanding of the mechanisms behind their associated toxicities.
NS: Are there biomarkers that can be used to stratify patients as either potential responders or non-responders to CAR-T cell therapy?
LB: Currently, we do not have any predictive biomarkers for patients and adoptive T cell and CAR-T cell therapy. We have interesting biomarker hits with tumor mutation burden and checkpoints because there have been so many patients treated and so much success with that therapy. I expect the same mechanisms of responsiveness to immune- based therapies may come up with adoptive transfer but we’re in earlier days than the checkpoint field. We’ll have to continue with hypothesis-generating high throughput analyses so that we can learn as much as possible. I think that predictive biomarkers will be the result of these studies.
NS: What are some of the biggest hurdles facing adoptive cell therapy for solid tumors?
LB: The tumor microenvironment itself is a challenge. In solid tumors, the cells need to infiltrate through the stroma and the immunosuppressive microenvironment in multiple sites and organs to find all the tumor cells. And don’t forget that the tumor has been established in the patient, sometimes for decades. The tumor has been edited and refined, the easily eliminated tumor cells have been winnowed out and what is left is in a mature, immunosuppressive environment that is not easily accessed by T cells. The cells have the potential to do the work but getting the T cells there and how to keep them functional are the two biggest hurdles.
NS: How likely is it that patients that are treated with adoptive cell therapy will have lasting immunological memory and protection from cancer in the future?
LB: The opportunity is there for durable responses and memory formation; in some patients, the effect has lasted for years. We’ve learned that treatment is not as effective when terminally differentiated cells are used; the younger, more stem cell-like cells may be more effective and have greater durability. We may need to design a mix of both effector cells and memory or stem cells to create an immediate therapeutic result and initiate a long-term protective effect. We know it is possible, but we don’t know how it has happened or how to control it.
NS: What adverse events are seen with treatment by adoptive T cell therapy and what can be done to minimize the side effects?
LB: Cytokine release syndrome, caused by the large amounts of secreted cytokines because of cell transfer, is the most common side effect. As a result, most therapeutic protocols require doses of IL-6 blocking antibody to be on hand. People are also looking upstream at the IL-1 family to see if blocking that pathway earlier might mitigate those symptoms. Neurotoxicity is another common side effect that is actively being investigated. Unfortunately, when something is useful there will be toxicity side effects, so we need to be prepared to deal with that. There are also instances of off-target reactions from T cell receptors that react with normal antigens as well as “on-target, off-tumor” toxicities, leading to the engineering of better regulated control switches into T cells. We can address the toxicity by controlling the T cell and revising the target.
NS: What are some of the bottlenecks in the manufacturing process of CAR-T cells in adoptive cell transfer?
LB: The manufacturing environment required individuals that are highly detail-oriented and capable of dealing with an extremely stressful environment. Bear in mind you are working with precious samples from cancer patients. If you mess up, you can’t just dump it in the trash and start fresh the next day because there might not be any more cells to use. We rely on GMP-grade (Good Manufacturing Practice) viral vectors and work under GMP conditions; these parameters are more expensive and time-consuming than what you do in a standard research lab. We in the field are partnering with the FDA to evaluate and streamline our processes. Patient safety is top of mind and yet there are some ways in which we can be nimbler to deliver results faster.
NS: Are new gene editing techniques like CRISPR being used in T cell engineering?
LB: This is a very exciting are to explore. It gives us the potential to edit out candidate molecules and edit in control switches. Gene editing and non-viral transfection methods will dramatically accelerate our ability to develop and test therapies.
NS: How do you think the field of adoptive cell transfer will benefit from NanoString’s new CAR-T cell panel?
LB: I expect this could open a lot of critical information about T cell biology. We may be able to look at our starting population of T cells from patients and correlate that profile with the previous treatments the patients have had. That will tell us about what their T cells can do. When that information is combined with their disease type and disease state we move to the next stage of assessing different manufacturing strategies and then select the appropriate way to move forward. We may have quantitative, reproducible data along the whole workflow of starting cells, manufactured cells, and infused cells. It’s even possible that we could track and pull cells back out of the patient and study what happened to the cells over time.
NS: What inspires you to keep pushing forward in what can be both an intellectually challenging and emotionally draining field?
LB: There are patients for whom none of the standard methods of treatment have been effective. When that patient is willing to roll the dice on an experimental treatment and then it works, allowing them to return to a normal life– that’s the best feeling in the world. It inspires me to keep exploring new options and improving our current practices. I want to keep increasing the percentages of durable, clinical responses from where we stand today to where I know the field can go.


